For many men, the prostate is a mysterious gland that only enters the conversation when something goes wrong. After 50, it moves from the background to the forefront of your health concerns. Talk of PSA tests, biopsies, and cancer risk can be confusing and anxiety-inducing.
The information out there is often conflicting. Some sources urge aggressive yearly testing, while others warn of the dangers of over-diagnosis. This leaves many men feeling paralyzed, unsure of what to do.
This guide cuts through the noise. It’s designed to empower you with clear, factual information about prostate health, explain the realities of screening, and equip you to have a productive, informed conversation with your doctor. Knowledge is the antidote to fear, and taking a proactive role is your best defense.
First, What Exactly is the Prostate and What Does It Do?
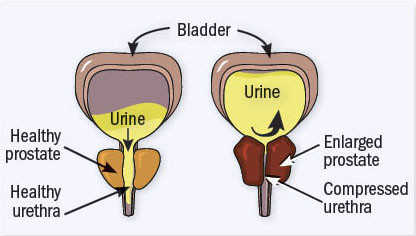
The prostate is a small, walnut-sized gland that sits below the bladder and surrounds the urethra (the tube that carries urine out of the body). Its primary function is to produce fluid that nourishes and transports sperm.
As men age, two common conditions can develop:
- Benign Prostatic Hyperplasia (BPH): This is a non-cancerous enlargement of the prostate. It’s extremely common, affecting about 50% of men by age 60 and up to 90% by age 85. It can cause bothersome urinary symptoms like frequent urination, a weak stream, or difficulty starting and stopping.
- Prostate Cancer: This is the uncontrolled growth of abnormal cells in the prostate gland. It is the most common cancer in men (after skin cancer), but it’s also often highly treatable, especially when detected early.
Crucial Point: Having BPH does not increase your risk of prostate cancer, nor does it turn into cancer. They are separate conditions that can happen at the same time.
Understanding the PSA Test: The Center of the Controversy
The Prostate-Specific Antigen (PSA) test is a simple blood test that measures the level of PSA, a protein produced by both normal and cancerous prostate cells.
- Why it’s useful: A higher-than-normal PSA level can be a red flag that indicates further investigation is needed. It helped revolutionize early detection.
- Why it’s controversial: The PSA test is not perfect. PSA levels can be elevated for many reasons other than cancer, including:
- BPH (the enlarged prostate itself produces more PSA)
- Prostatitis (an infection or inflammation of the prostate)
- Recent ejaculation
- A urinary tract infection
- Even a long bike ride
This can lead to false positives—an elevated PSA that triggers anxiety and invasive tests (like a biopsy) that ultimately find no cancer.
The other side of the coin is over-diagnosis. The test can find very slow-growing, low-risk cancers that would never have caused symptoms or harm in a man’s lifetime. Treating these cancers (with surgery or radiation) can lead to significant side effects like urinary incontinence and erectile dysfunction, meaning men can be harmed by treating a cancer that didn’t need to be treated.
So, Should You Get a PSA Test? A Framework for Decision Making
This is not a simple yes or no question. It’s a personal decision you should make in partnership with your doctor, based on your individual risk profile.
Step 1: Understand Your Risk Factors
- Age: Risk increases significantly after 50.
- Race: African American men have a higher risk of developing and dying from prostate cancer.
- Family History: Your risk doubles if you have a father or brother who had prostate cancer. It’s even higher if they were diagnosed at a young age.
Step 2: Know the Guidelines
Major health organizations have slightly different guidelines, but they all emphasize shared decision-making. This means your doctor should explain the potential benefits and risks, and you decide together what’s right for you.
- For men at average risk (no family history, not African American), discussions about screening often begin at age 50.
- For men at higher risk (African American or with a family history), discussions often begin at age 45.
- For men at very high risk (multiple family members diagnosed young), discussions may begin at age 40.
Step 3: Ask Yourself and Your Doctor These Key Questions
Before you decide, have a conversation. Go in prepared.
- “Based on my age and risk factors, what do you recommend?”
- “If my PSA is high, what are the next steps?”
- “What are the potential benefits of finding prostate cancer early for a man my age?”
- “What are the risks of a false positive or over-diagnosis?”
- “If a low-risk cancer is found, what are my options besides immediate treatment?” (Active surveillance is a common and valid approach for low-risk cases).
Beyond PSA: Symptoms You Should Never Ignore
While screening is for finding cancer before symptoms appear, you should see a doctor immediately if you experience any of these, as they can be signs of BPH or advanced prostate cancer:
- Difficulty urinating or a weak/interrupted urine flow
- A frequent or urgent need to urinate, especially at night (nocturia)
- Blood in the urine or semen
- Pain or a burning sensation during urination or ejaculation
- Persistent pain in the back, hips, or pelvis
These symptoms are most likely due to BPH, but they require a professional diagnosis.
The Bottom Line: Be Proactive, Not Paranoid
Your prostate health is a key part of your overall well-being after 50.
- Don’t avoid the conversation. Bring it up at your next physical.
- Educate yourself on your personal risk factors.
- Engage in shared decision-making with your doctor about the PSA test. There is no one right answer for every man.
- Report any urinary or pelvic symptoms to your doctor promptly.
By being informed and engaged, you can move from a place of anxiety to a place of empowerment, ensuring you make the best choices for your long-term health.
FAQ Section
Q: What is a normal PSA level?
A: Traditionally, a PSA level below 4.0 ng/mL was considered normal. However, this is not a hard rule. A more important factor for your doctor is the PSA velocity—how quickly your PSA level rises over time. A jump from 1.0 to 3.0 is more concerning than a stable level of 3.5.
Q: What happens if my PSA level is high?
A: Don’t panic. It does not mean you have cancer. Your doctor will first rule out other causes like infection. They may recommend repeating the test. If it remains high, the next step might be an MRI of the prostate to get a clearer picture, which can then help decide if a biopsy is necessary.
Q: What is active surveillance?
A: For men diagnosed with very low-risk or low-risk prostate cancer, active surveillance is a management strategy. Instead of immediate treatment (like surgery or radiation), the cancer is monitored closely with regular PSA tests, digital rectal exams (DREs), and occasional biopsies. Treatment is only recommended if the cancer shows signs of progressing. This avoids the side effects of treatment for cancers that may never cause harm.
Q: Are there ways to support prostate health naturally?
A: While no magic food prevents cancer, a heart-healthy diet is also a prostate-healthy diet. Some evidence suggests foods rich in lycopene (cooked tomatoes, watermelon), cruciferous vegetables (broccoli, cauliflower), and healthy fats (fish, nuts) may support prostate health. Staying active and maintaining a healthy weight are also beneficial.